Confusion between Medicare and Medicaid can result in thousands of dollars in uncovered medical bills for families. While the names sound alike, these two government programs serve different purposes, cover different services, and have vastly different rules.
For many seniors, the most surprising fact isn't what Medicare includes but what it excludes, such as long-term nursing home care and regular dental services. Understanding the differences between Medicare and Medicaid is crucial for protecting your health and financial well-being.
Key Takeaways:
- Medicare is typically available to individuals aged 65 and older, regardless of their income level.
- Medicaid is designed for individuals with limited income and assets.
- Dual Eligibility: You can have both at the same time, which covers almost all costs.
- The "Gap": Medicare rarely covers dental, vision, or long-term custodial care; Medicaid often does.
- Transportation: Medicaid offers free rides (NEMT), but services like GoGoGrandparent offer a more reliable alternative.
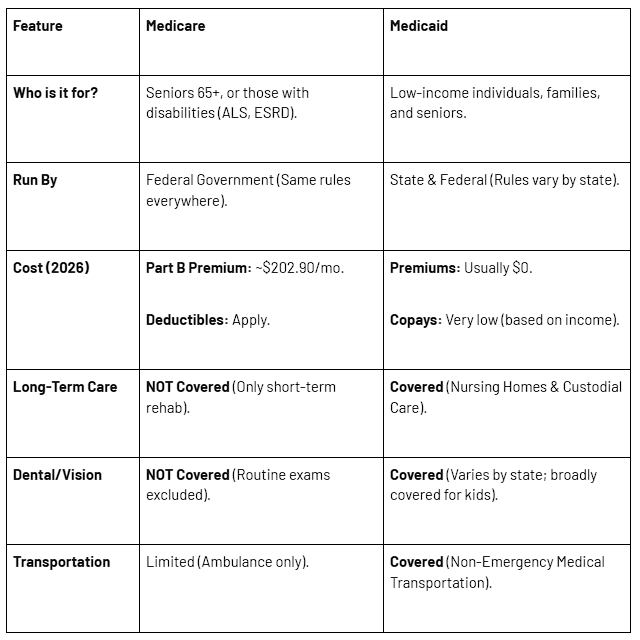
The Quick Comparison Table
If you need a fast answer, this table breaks down the core differences for 2026.
Can You Have Both? The Guide to Dual Eligibility
One of the most common questions we hear is: "Can you have both Medicare and Medicaid?"
Yes. If you qualify for both, you are considered "Dual Eligible."
This is the "gold standard" of coverage. Here is how it works:
- Medicare pays first: It covers your doctor visits and hospital stays.
- Medicaid pays second: It steps in to pay the costs Medicare leaves behind, such as the 20% coinsurance and the Part B premium.
Dual Eligible Special Needs Plans (D-SNPs)
If you are dual eligible, you may qualify for a Dual Eligible Special Needs Plan (D-SNP). These are specialized Medicare Advantage plans that coordinate your care between the two programs. They often include extra benefits like:
- Credits for healthy food and utilities (subject to new 2026 verification rules).
- $0 copays for prescription drugs.
- Care coordination to help you manage appointments.
Note on 2026 Changes: Starting in 2026, the "Value-Based Insurance Design" (VBID) model will end. This means D-SNPs will have stricter rules for offering grocery cards; you may need to verify a chronic condition to qualify for these specific perks.
The Coverage Gap: Dental, Vision, & Long-Term Care
Original Medicare is excellent for "acute" care (such as a heart attack or the flu), but it has significant gaps when it comes to "chronic" or "maintenance" care.
1. The Dental, Vision, & Hearing Gap
Original Medicare does not cover routine dental checkups, cleanings, dentures, or implants. It also excludes routine eye exams for glasses and hearing aids.
- Medicaid's Role: Medicaid can fill this gap, but it depends on your state. States like New York and California have expanded adult dental coverage, but many other states limit coverage to emergencies only.
- Important: Does Medicaid usually cover dental implants? Typically, no. Since implants are often classified as "elective," Medicaid generally only covers dentures.
2. The Nursing Home Myth
Many families assume that Medicare will cover the costs of a nursing home. It does not.
- Skilled vs. Custodial Care: Medicare only pays for "Skilled Nursing" (rehab) for up to 100 days after a hospital stay. It pays $0 for "Custodial Care" (help with activities of daily living, such as bathing, dressing, and eating).
- Medicaid's Role: Medicaid is the primary payer for long-term custodial care in the U.S. To qualify, seniors often have to "spend down" their assets to meet strict limits (typically around $2,000 for an individual).
Getting to the Doctor: Transportation Benefits
A great doctor is of little use if you cannot reach their office. This is where the logistical differences between Medicare and Medicaid become apparent.
Medicaid includes a federally mandated benefit called Non-Emergency Medical Transportation (NEMT). This provides free rides to medical appointments for beneficiaries who have no other means of transportation.
The Problem with NEMT:
While free, Medicaid transportation is famously difficult to navigate.
- Advance Notice: You often must book rides 48–72 hours in advance.
- Wait Times: Seniors report waiting hours for a return ride after their appointment.9
- Shared Rides: You may be in a van with several other patients, making a short trip take hours.
The Reliable Alternative: GoGoGrandparent
For seniors seeking independence and reliability without the hassle of NEMT, GoGoGrandparent provides reliable medical transportation.
- On-Demand: No need to book days in advance.
- Monitored: Our "GoGoGuardians" monitor the ride 24/7 to ensure safety.
- No Smartphone Needed: You can book with a simple phone call.
If you don't qualify for NEMT or simply need a better experience, we can help you get there.
2026 Medicare & Medicaid Costs
Planning your budget requires staying up-to-date with the latest numbers. Here are the official figures for 2026:
Medicare Costs (2026)
- Part B Premium: The standard monthly premium is $202.90 (up from 2025).
- Part B Deductible: $283 per year.
- Part A Deductible: $1,736 per hospital benefit period.
Medicaid Costs (2026)
- Premiums: Generally $0 for those under the income limits.
- Income Limits: Eligibility varies by state, but for the Qualified Medicare Beneficiary (QMB) program (which pays your Medicare premiums), the monthly income limit is approximately $1,325 for an individual (100% FPL + $20 disregard).
- Asset Limits: Most states limit assets to $2,000. Crucial Update: California (Medi-Cal) has reinstated asset limits effective January 1, 2026, set at $130,000 for an individual.
State-Specific Medicaid Names
Medicaid goes by many names. If you are looking for application forms, search for your state's specific program name:
How GoGoGrandparent Bridges the Gap
Navigating insurance is hard enough; living independently shouldn't be. Whether you have Medicare, Medicaid, or are Dual Eligible, GoGoGrandparent helps you utilize your benefits and fill the gaps.
- Prescription Delivery: We offer a service that works with your pharmacy to get your meds to your door—vital for those with mobility issues.
- Groceries & Meals: If your D-SNP food benefits change in 2026, our operators can help you find affordable meal delivery options.
- Rides: We provide the freedom to travel on your schedule, not the bus schedule.
Frequently Asked Questions (FAQ)
1. Do I lose Medicare if I get Medicaid?
No. You keep both. Medicare pays first, and Medicaid pays second. This "Dual Eligible" status covers most of your costs.
2. Does Medicaid cover dental implants in 2026?
Generally, no. While some states, such as New York, have expanded dental coverage, implants are rarely covered unless medically necessary for reconstruction purposes. Most states cover dentures and extractions.
3. What is the Medicaid "Look-Back" period?
When you apply for long-term care Medicaid (nursing home) benefits, the state reviews your finances for the past 5 years (or 30 months in California). If you gave away money or assets during this time, you may be penalized.
4. Why is my Part B premium higher than $202.90?
If your income exceeds $109,000 as an individual or $218,000 as a couple, you will be subject to an additional surcharge known as IRMAA.


